On January 11, 2018, the Center for Medicare and Medicaid Services (CMS) released new guidance for states considering a Medicaid work requirement. One day later, Kentucky became the first state to get federal approval to add a work requirement (although legal challenges appear likely).
These developments help answer some of the questions raised in Part 3 of our introductory series on Medicaid work requirements and create additional issues for policymakers to consider. Below, we break down and analyze the guidance from CMS and then look at 7 key elements of Kentucky’s waiver.
Analyzing the New Guidance from CMS
Work Requirement Goals
Work requirements “should be designed to promote better mental, physical, and emotional health” of Medicaid enrollees, according to the guidance from CMS. States may also set additional goals like helping individuals “attain independence.” (1) States will have to track outcomes towards these goals (see below).
Affected Populations
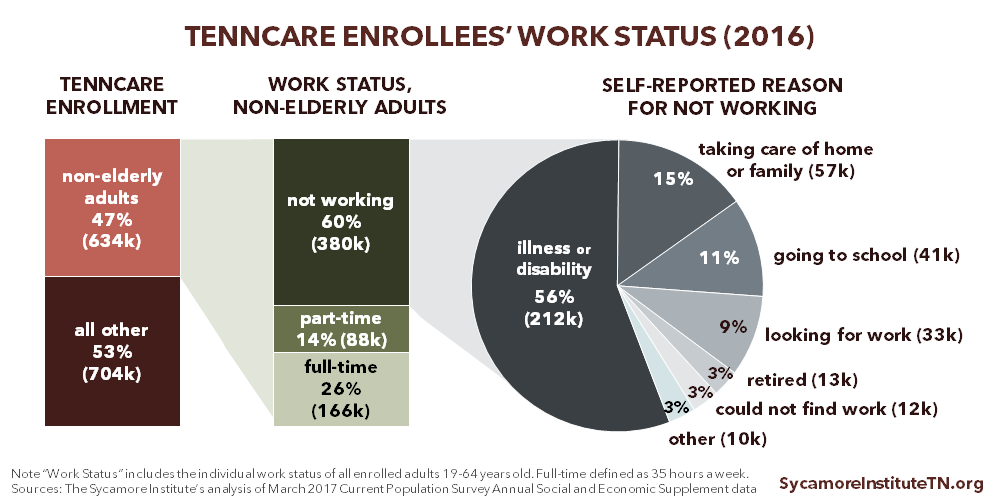
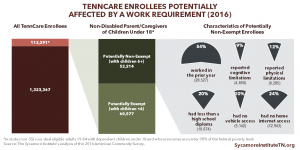
Medicaid work requirements can only be applied to “non-elderly, non-pregnant adult beneficiaries who are eligible for Medicaid on a basis other than disability.” Other adults with illnesses that prevent them from complying with work requirements (as determined by a doctor) must be exempt. Additionally, states are expected to either exempt people with substance use disorders or modify requirements to ensure access to Medicaid coverage and treatment. (1) Because Tennessee did not participate in the Affordable Care Act’s optional Medicaid eligibility expansion, few childless adults without disabilities are eligible for TennCare. Policymakers weighing the trade-offs of a TennCare work requirement may want to consider the size of the affected population as they balance the potential costs and benefits.
*These data rely on a national survey and not TennCare program data, and they lack key details about enrollees’ individual circumstances. Part 1 of our introductory series discusses the limitations of these data in greater detail.
Definition of Work
CMS encouraged states to define “work” broadly. Job training and support services, career planning, volunteering, substance abuse treatment, and caring for young children and elderly family members may be considered as countable work activities. (1) CMS also expects states to consider structural barriers (e.g. local labor market, transportation) that may make it difficult for enrollees to comply with requirements. Policymakers may consider how they will define work and address structural barriers to employment.
Support Services
Federal Medicaid dollars cannot be used to pay for support services. Support services like child care, transportation, education and job training help address employment barriers and are a major component of traditional welfare-to-work programs. (2) For example, support services make up nearly half of Tennessee’s Families First budget. CMS requires that states outline the strategies they will use to help enrollees meet work requirements, including linking individuals to support services. However, states cannot use federal Medicaid match dollars to finance these services. (1) The capacity to fund support services may significantly affect a state’s ability to achieve the goal of a Medicaid work requirement.
Coordination with Other Programs
CMS encouraged states to align Medicaid work requirements with existing work requirements for the Supplemental Nutrition Assistance Program (SNAP) and Temporary Assistance for Needy Families (TANF). SNAP and TANF enrollees who comply with or are exempt from those work requirements must be considered to have met any Medicaid work requirement. (1) States must also tell people how the requirements change if they leave SNAP or TANF but remain on Medicaid. Such alignment between programs would take significant interagency coordination and could raise administrative costs. Integrated eligibility systems may ease some of that burden. Policymakers might consider if and how TEDS — a new eligibility determination system being developed for TennCare — would coordinate with Families First (Tennessee’s TANF program) and SNAP.
Tracking Outcomes
States must track health and employment outcomes to evaluate the effect of work requirements. CMS requires an extensive evaluation and monitoring plan with independent program evaluations and follow-ups with people who leave Medicaid due to employment or failure to meet work requirements. (1) Collecting data on health and employment outcomes for non-exempt enrollees would likely demand significant case management services. Part 2 of our introductory series looks at the integration of a work requirement and related services into an existing program (Families First) and the challenges of longer-term evaluations of individuals who leave public programs.
Budget Neutrality
States must demonstrate that a work requirement does not increase program costs. Certain elements of Medicaid work requirements — to be determined by CMS and each state — must be budget neutral, and states cannot count savings from any drop in enrollment due to the requirement. (1) Challenges to achieving budget neutrality could potentially include the administrative costs of interagency coordination and effective tracking, monitoring, and evaluation.
Key Elements of Kentucky’s Medicaid Work Requirement
Kentucky expanded Medicaid in 2014. According to its waiver application, the state expects work requirements to lower the costs of its expansion population and improve health outcomes and quality of life for all its Medicaid enrollees. (4) (5) The demonstration project just approved by the feds, called Kentucky HEALTH, will serve as a learning opportunity for Tennessee and other states thinking about a Medicaid work requirement.
Here are 7 important components of the program plus one additional project included in Kentucky’s waiver.
1. Aims to Transition Enrollees to Private Insurance
A major goal of the project is transitioning certain Medicaid enrollees into the commercial health insurance market. Kentucky HEALTH primarily affects the Medicaid expansion population but also includes other children and non-disabled adults. The demonstration includes work requirements, premiums and deductibles, health care spending accounts, and premium assistance for employer-sponsored insurance. (5)
2. Affects Able-Bodied Adults without Dependents
All able-bodied adults aged 19-64 years of age without dependents are subject to the work requirement. Exempt populations include: children, pregnant women, individuals determined medically frail, and adults who are the primary caregiver of a dependent (i.e. minor child or adult with a disability).
3. Gradual Phase-In for Enrollees
Work requirements will phase in gradually. During their first 3 months in the program, enrollees must complete at least 5 hours of employment or community engagement activities. By 12 months, all able-bodied adults must engage in at least 20 hours per week. Kentucky may phase in the requirements by county or region to ensure adequate resources for enrollees and to monitor the program. (5)
4. Broad Definition of Work
Work is broadly defined. Countable work activities include:
- Job skill training and search activities.
- General education, vocational education/training, and education related to employment.
- Community service and work experience.
- Caregiving for a non-dependent relative or other person with a chronic, disabling health condition.
Full-time students and people already working at least 20 hours a week will automatically meet the work requirement and will not need to participate in additional activities. (5)
5. Eligibility Depends on Work
Kentucky HEALTH ties work requirements to Medicaid eligibility. Medicaid eligibility will suspend if enrollees do not comply with the work requirement. To get suspended benefits reinstated, enrollees must complete 80 hours of community engagement in a 30-day period or a state-approved financial literacy or health literacy course. Benefits will be reinstated on the first day of the month after they complete community engagement activities or state-approved courses. Those who do not comply by the deadline will be disenrolled from Medicaid. If they desire to reenroll, they must reapply. (3)
6. Incentives and Support Services Encourage Compliance
Kentucky HEALTH will use incentives and support services to encourage compliance with work requirements. Enrollees will get credits in a health care savings account if they engage in more countable work activities than required. These credits can help pay any required premiums and deductibles. The Kentucky Cabinet for Education and Workforce Development will also work with Medicaid enrollees to provide support services and help them meet the work requirement. (5)
7. County-by-County Rollout
Kentucky will assess each county’s capacity to implement the work requirement. Kentucky plans to assess the adequacy of job training, employment, and community engagement resources for enrollees in each county before implementing the requirement in that county. This is intended to help ensure that non-exempt enrollees can meet their work requirements. This gradual phase-in will also provide a natural experiment to evaluate the impact of the work requirement.
BONUS: Effort to Address Mental Substance Abuse & Mental Health
Separate from the work requirement, Kentucky’s federal waiver also approved a pilot project to increase access to substance abuse and mental health services. Kentucky plans to identify high-need counties and pilot a program to improve the mental health and substance abuse delivery system and address prescription drug and opioid abuse. This pilot project will not affect existing Medicaid benefits for mental health and substance abuse. (5)
Related Work by The Sycamore Institute
Medicaid Work Requirements in Tennessee
(September – December 2017) A 3-part introductory series.
Medicaid Eligibility in Tennessee
(August 30, 2017) A summary of how TennCare eligibility is determined.
Understanding Medicaid and TennCare: Key Concepts and Context to Know
(June 1, 2017) An overview of the program’s goals, history, function, structure, funding, and cost drivers.
References
Click to Open/Close
- Department of Health and Human Services. RE: Opportunities to Promote Work and Community Engagement AMong Medicaid Beneficiaries. Center for Medicare and Medicaid Services. [Online] January 11, 2018. [Cited: January 12, 2018.] https://www.medicaid.gov/federal-policy-guidance/downloads/smd18002.pdf.
- Musumeci, MaryBeth and Zur, Julia. Medicaid Enrollees and Work Requirements: Lessons From the TANF Experience. Kaiser Family Foundation. [Online] August 18, 2017. [Cited: November 30, 2017.] https://www.kff.org/medicaid/issue-brief/medicaid-enrollees-and-work-requirements-lessons-from-the-tanf-experience/.
- Department of Health and Human Services. Approval Package for Commonwelath of Kentucky’s section 1115 demonstration project. Center for Medicare and Medicaid Services. [Online] January 12, 2018. [Cited: January 12, 2018.] https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ky/ky-health-ca.pdf
- Kaiser Family Foudation. Proposed Changes to Medicaid Expansion in Kentucky. [Online] August 4, 2017. [Cited: January 12, 2018.] https://www.kff.org/medicaid/fact-sheet/proposed-changes-to-medicaid-expansion-in-kentucky/.
- Commonwealth of Kentucky, Office of the Governor. Kentucky HEALTH Section 1115 Demonstration Application. [Online] August 24, 2016. [Cited: January 2018, 2018.] https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ky/ky-health-pa.pdf.