There’s a complicated relationship between public health and public policy. 5 Ways Public Policy Impacts Health explains how government actions or inaction — even in areas not always considered health-related — can impact people’s health. The opposite is also true…Tennesseans’ health can affect our state’s ability to achieve many policy goals. For example, policies aimed at economic opportunity can influence health, but good health is also associated with higher worker productivity. This means that Tennesseans’ health has an effect on Tennessee’s economic prosperity. (1) (2)
These relationships often overlap and influence one another, which makes the challenging task of developing effective public policy even harder. Fortunately, approaches to policymaking that recognize and account for these complex interactions can make the task easier. Below, we summarize two examples of cross-cutting policy approaches with successful track records.
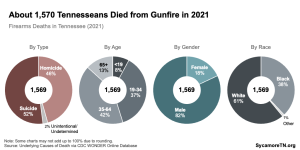
Health in All Policies
The “Health In All Policies” approach is one way to routinely consider the health impact of all public policies. Developed by the public health community, the approach recognizes that all stakeholders have something to gain from changing how public agencies work together and how public policy decisions are made.
The Health In All Policies approach often uses Health Impact Assessments (HIA) as a tool to collect data, engage different stakeholders, and determine short- and long-term impacts of a proposed effort. (3) In Tennessee, the Knox County Health Department, the Memphis and Shelby County Office of Sustainability, the Tennessee Obesity Taskforce, and the Nashville Metropolitan Planning have all used HIAs in their policymaking processes. (4)
 Integrated Services
Integrated Services
Another method is the “integrated services” approach, which focuses on public programs that integrate and connect clinical care with other services that impact health.
Home Visits
Home visiting programs are a good example of an integrated service that has proven successful at addressing multiple drivers of health through a single point-of-entry (i.e. a home visit). The programs pay for trained professionals in health, social work, and/or education to visit the homes of low-income pregnant women, infants, and young children to provide guidance and assistance.
Such programs have shown positive results for a number of social and economic factors that can influence a child’s health, development, school readiness, and long-term outcomes. For example, home visiting programs may help mothers with education and employment goals, connect families to other community resources, and reduce exposure to crime by addressing domestic violence. (5) Tennessee funds evidence-based home visiting programs in 51 counties in the state. (6) Maternal and infant home visiting programs first received federal funding in 2010.
Similar programs focused on ensuring the safety of Medicare patients’ homes and helping elderly patients take better care of themselves have shown promise in maximizing the effectiveness of clinical care. (7)
Clinically-Driven Programs
Another example of integrated services are clinical approaches that directly address the drivers of health. Some hospital systems, for example, are working to connect high-cost patients with non-clinical needs, like food and housing. (8)
In 2016, the federal Centers for Medicare and Medicaid Services (CMS) launched the Accountable Health Communities pilot project. The project funds the infrastructure and staff needed to connect Medicaid enrollees with non-clinical needs like housing, food, utilities, and transportation. It will ultimately measure whether and to what extent these activities improve health outcomes and/or save taxpayer dollars. Thirty-two organizations nationwide are participating — including Mountain States Health Alliance in Johnson City. (9)
Parting Words
All policy decisions have trade-offs. As our state’s policymakers weigh these trade-offs, they should also consider how policies will affect the health and well-being of Tennesseans and, in turn, how the health and well-being of Tennesseans will affect a broad range of policy objectives.
References
Click to Open/Close
1. Schultz, Alyssa, Chen, Chin-Yu and Edington, Dee. The Cost and Impact of Health Conditions on Presenteeism to Employers. Pharmacoeconomics. [Online] May 2009. http://link.springer.com/article/10.2165/00019053-200927050-00002.
2. Mitchell, Rebecca and Bates, Paul. Measuring Health-Related Productivity Loss. Population Health Management. [Online] April 2011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3128441/.
3. Rudolph, Linda, et al. Health In All Policies: A Guide for State and Local Governments. American Public Health Association and Public Health Institute. [Online] 2013. https://www.apha.org/~/media/files/pdf/factsheets/health_inall_policies_guide_169pages.ashx.
4. Tennessee Department of Health. Health Impact Assessment. [Online] 2017. https://www.tn.gov/health/cedep/environmental/healthy-places/healthy-places/tools-and-resources/tr/hia.html
5. U.S. Department of Health and Human Services. Demonstrating Improvement in the Maternal, Infant, and Early Childhood Home Visiting Program: A Report to Congress. [Online] March 2016. https://mchb.hrsa.gov/sites/default/files/mchb/MaternalChildHealthInitiatives/HomeVisiting/pdf/reportcongress-homevisiting.pdf.
6. Tennessee Department of Health. Evidence Based Home Visiting Programs. [Online] 2017. https://www.tn.gov/health/health-program-areas/fhw/early-childhood-program/evidence-based-home-visiting-programs.html
7. Ruiz, Sarah, et al. Innovative Home Visit Models Associated with Reductions in Costs, Hospitalizations, and Emergency Department Use. Health Affairs. [Online] March 2017. http://content.healthaffairs.org/content/36/3/425.short.
8. O’Donnell, Jayne. Hospitals Target Nutrition, Other Social Needs to Boost Health. USA Today. [Online] February 17, 2017. https://www.usatoday.com/story/news/politics/2017/02/17/hospitals-target-nutrition-other-social-needs-boost-health/98042112.
9. Centers for Medicare and Medicaid Services. Accountable Health Communities Model. U.S. Department of Health and Human Services. [Online] 2017. https://innovation.cms.gov/initiatives/ahcm/.